10 Sexually Transmitted Diseases You Didn’t Know Existed
Over one million sexually transmitted diseases are acquired everyday according to the World Health Organization. With a number so high, it goes without saying that STD education is important. Often times, when the topic of STDs comes up, diseases like gonorrhea, herpes, and chlamydia get the spotlight. And with good reason. They are among the most common sexually transmitted diseases. However, there are about 20 sexually transmitted diseases, and a lot of them don’t get as much attention. Yet they are either comparably common or important to know about. Here, we will explore 10 of those diseases, their symptoms, and their treatment.

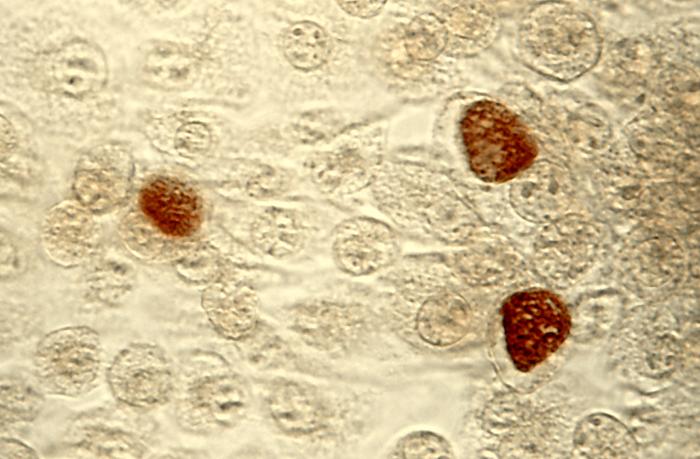
1. Mycoplasma genitalium
The bacterium Mycoplasma genitalium (or M. gen for short) was first identified in 1981 in men who suffered from the inflammation of the urethra (a.k.a. urethritis). Despite not being as well-known, M. gen’s prevalence has surpassed that of gonorrhea. Doctors believe that this sexually transmitted disease infects 1 to 3 percent of people. Yet surprisingly, many people with M. gen don’t realize they have it! But if symptoms do show, the male reproductive system could release penile discharge that has a watery consistency. Because of M. gen’s link to urethritis in men, symptoms could also include painful urination. In the female reproductive system, M. gen could cause in vaginal discharge, painful periods, bleeding, between periods, and pain during sex. M. gen may also cause infertility in the female reproductive system.
Diagnosis of M. genitalium
To date, there is no FDA-approved treatment for M. gen. However, if the doctor notices that the patient has urethritis or cervicitis and other STDs like chlamydia and gonorrhea have been ruled out, the doctor may choose test for M. gen. Nucleic-Acid Amplification Testing (or NAAT) is the method of choice. The patient gives the health professional a urine sample and NAAT works by identifying DNA in the sample that matches that of M. gen. Once detected, the patient can move on to treatment.

[Photo Credit: Thomas Deerinck, NCMIR/Science Source.]
Treatment of M. genitalium
Azithromycin and doxycycline are the drugs that treats M.gen. However, there has been growing evidence that M.gen is antibiotic resistant, meaning that more of the bacteria lingers in the body and becomes less affected by antibiotics. Consider what this doctor observed in those who needed antibiotic treatment:
Dr. Goje noted that patients who have not responded to an initial course of doxycycline often require a second round of antibiotic treatment, usually consisting of azithromycin for at least 5 days. However, up to 50% of patients with M. genitalium infection exhibit resistance to azithromycin. In cases of azithromycin failure, moxifloxacin 400 mg daily for 7 to 14 days is the preferred antibiotic regimen. “Cure rates with moxifloxacin are 100% in initial reports, although more studies are needed,” Dr Goje said.
from “Mycoplasma genitalium: Challenges in Diagnosis and Treatment” by Crystal Wong, MD
2. Lymphogranuloma Venereum (LGV)
LGV happens when the lymphatic system is infected. Three rare strains of the Chlamydia trachomatis bacteria cause LGV (not including the one that causes the STD Chlamydia). LGV tends to occur in sexually active people who live in tropical and subtropical climates. It does not occur as much in the Western world. However, incidences have occurred among sexually active people in the UK and in the Southern region of the United States.
LGV can be transmitted vaginally, anally, and orally. It’s possible that LGV occurs in men and women equally. However, it is easier to spot in men than women early on. Because of this, men report having the disease more often than women. In women, the disease manifests itself much later in its lifespan. It is also common for complications to arise during this later time period.
Symptoms, Diagnosis, and Treatment of LGV
Symptoms of LGV include small, painless sores on the genitals and redness and swelling of the groin. Since LGV infects the lymphatic system, one may experience the swelling and/or drainage of lymph nodes in the groin. When transmitted anally, LGV can also cause swelling in the lymph nodes around the rectum. The disease can result in bloody stools and painful bowel movements. In the female reproductive system, LGV can include the swelling of the labia.
After the symptoms have manifested themselves, doctors can take the biopsy or blood sample from the affected area and test for the presence of LGV. Once diagnosed, the infected person can take their prescribed antibiotic to treat the LGV. The antibiotic of choice tends to be doxycycline or erythromycin.
3. Chancroid
The sinister Haemophilus ducreyi bacteria causes the Chancroid STI. This infection gets its name from the sores, called chancroids, that can appear in the genital area when one is infected. It is more common outside of North America and Europe. However, random outbreaks of the infection have occurred in the United States though the prevalence of the disease has declined as a whole.

[Source: Wisconsin Department of Health Services]
Symptoms, diagnosis, and treatment of Chancroid
Most people infected with Chancroid will experience symptoms though it is possible for some people to be asymptomatic. The symptoms are primarily ulcers that can show up within a day to over a week after infection. The sores are small and painful with sharply defined borders. Their base has a yellowish, grayish color. They also can easily bleed if scratched. It is also possible to experience painful urination, swollen lymph nodes, and/or a swollen groin when infected.
To confirm if someone has chancroid, a healthcare provider can examine the ulcers and see if the person has swollen lymph nodes. Alternatively, the healthcare provider can take cells from where they think the patient is infected and grow it in a cell culture. As it grows, they will be on the look out for the H. ducreyi bacteria. If it shows up, then the person has chancroid.
The downside is that this test isn’t widely available. And even if used, the sensitivity to the bacteria is less than 80%. Not the greatest effectiveness, I’m afraid. Also, in the U.S., the Center of Disease Control states that there is no FDA-approved test. Thankfully though, there are labs with their own CLIA verified tests.
If the lymph nodes are large, the healthcare provider may drain them with a needle or via surgery. To fight the infection, the healthcare provider can prescribe antibiotics such as azithromycin and ceftriaxone.
4. Donovanosis
The bacterium Klebsiella granulomatis is the troublemaker that causes donovanosis. It is common in tropical and subtropical countries, occurring mainly in 20 to 40 year olds. And it is primarily spread anally and vaginally. It’s not typically transmitted orally. After one comes in contact with the disease, symptoms can start anywhere from 1 to 12 weeks later.
Chancroid and donovanosis look similar when observed in their early stages. And like chancroid, donovanosis causes the infected person to develop ulcers. However, donovanosis ulcers produce raised, red, fleshy bumps on or around the genital and anal regions respectively, resulting in granulation tissue. If left untreated, the disease will be destructive, slowly spreading and damaging genital tissue, possibly even spreading to the groin. The sores can also bleed if scratched and can produce a putrid odor if bacteria infects these sores. In its later stages, Donovanosis resembles LGV and advanced genital cancer.
In order to diagnose someone who may have the infection, the healthcare provider can take a tissue sample of the ulcer or take a blood test to see if Donovanosis or other STDs are present. If the test is positive, the healthcare provider can prescribe antibiotics.

5. Cytomegalovirus
Unlike the sexually transmitted diseases we have talked about so far, cytomegalovirus (or CMV) is a common viral infection. It belongs to the same viral family as cold sores (HSV 1) and genital herpes (HSV 2).
Like cold sores, CMV also infects people outside of sexual contact. Beyond semen and natural lubrication fluid, CMV can also be transmitted via other bodily fluids. These include saliva, blood, urine, breastmilk, and amniotic fluid. And, as you might have guessed, CMV can be passed from an infected pregnant woman to her unborn child. This is called Congenital CMV. CMV can also be passed during birth or right after birth, usually once the baby has their first feed of breastmilk. This is called Perinatal CMV.
Given how common CMV is, 1 in 200 babies born in the United States contract CMV. However, of the babies born with CMV, only 1 in 5 experience the long term effects of the viral disease. An unfortunate truth is that CMV is also the leading infection to cause miscarriages.
Symptoms and Treatment of CMV
CMV is also closely related to mononucleosis, commonly referred as “mono” for short. As a result, when symptoms show, they are quite similar to that of mono. They include muscle aches, fatigue, fever, and a sore throat. Thankfully, most adults will not experience any symptoms. This is also true for a number of newborns. However, when newborns show signs of infection, they can have jaundiced skin, a rash, low weight, seizures, damaged eye retinas, and/or an enlarged liver or spleen among other things.
Much like cold sores and genital herpes, there is no cure for CMV. However most children and adults typically recover from symptoms without medication. Unfortunately, some children develop long-term issues and need treatment. Those issues include hearing loss/impairment, vision loss, seizures, developmental and motor delay, and/or a smaller sized head. Doctors can prescribe such patients antiviral medication like Valganciclovir which may treat developmental and hearing issues.
Given cytomegalovirus’ prevalence in the population during childhood, a number of health professionals hesitate from calling it an “official STD” while others consider it an STD. But what is very clear is that it can very well be sexually transmitted.
6. Nongonoccocal Urethritis (NGU)
NGU occurs when something other than gonorrhea infects the urethra. While a variety of bacteria can cause NGU, the common culprit is Chlamydia trachomatis. NGU is most common in men, especially those ages 15 to 30 who have had multiple sexual partners. However, women can acquire the infection, too. Also, NGU can be passed anally, vaginally, or orally with an infected person.
[Source: CDC]
Though NGU infects people primarily via sexual contact, one can get it via nonsexual ways like urinary tract infections or even when a catheter is inserted. If a pregnant woman has NGU and she delivers her baby, she can also pass the infection on to her newborn.
It is common for those infected with NGU to feel a burning sensation when urinating. Discharge from the penile or vaginal area is also a common symptom. Penile itching and irritation can occur and so can abnormal vaginal bleeding or abnormal abdominal pain. In fact, that pain might indicate that the NGU infection has progressed to Pelvic Inflammatory Disease.
Beyond physical signs of the disease, the health care provider can take samples of the infected area and check for bacteria other than gonorrhea. They may also analyze urine samples (though that is rare).
Once diagnosed, the doctor can prescribe the patient antibiotics like azithromycin and doxycycline.
7. Scabies
Now scabies is unlike every STD we have talked about so far. Scabies is not an infection. It is an infestation. Unlike an infection, scabies occurs when parasitic, insect-like, microscopic organisms called itch mites burrow into the skin of its host, causing the individual a great deal of discomfort. Scabies causes rashes that look like small red bumps and blisters. This makes the affected person prone to scratching themselves. This scratching may, unfortunately, make the individual prone to secondary diseases.

[Source: Wikipedia Commons]
Scabies has shown itself in human bodies for more than 2,500 years. In addition, 300 million cases are reported worldwide every year. While scabies is mainly sexually transmitted among sexually active people, it can also be transmitted in nonsexual skin-to-skin contact with the affected area. While it does show up in the genital and anal area, it can also be found in the lower fold of skin between the fingers, the wrist area, and the backs of the elbows. Scabies can also show itself around one’s waist and belly button and in the knee area.
Ironically enough, it is not unheard of that scabies breakouts occur in nursing homes, hospitals, and nursing home facilities. This is because the physical manifestation of scabies is not as apparent as it is in younger populations, so skin contact with them can happen more easily. Scabies is also common among the homeless.
Diagnosis of Scabies
Beyond the red rashes, a health practitioner may want to take a sample of the affected area and put it underneath the microscope to check for the presence of the mites. If diagnosing is difficult, PCR testing is an option and it will give the healthcare provider the genetic material of the scabies mites; this isn’t a common method though.
Once the health professional confirms that the infected individual has scabies, the health professional can prescribe scabicide creams or oral medication.
Given how unique scabies is, it’s important to note that barrier methods of protection (like condoms) won’t work with this one. If you and your partner contract it, it is important that both of you get treatment so you all aren’t just passing it back and forth sexually or non-sexually.
8. Pelvic Inflammatory Disease (PID)
PID is an STD exclusive to the female reproductive system. It occurs when bacteria spreads from the vagina upward, infecting the uterus, fallopian tubes, and/or ovaries. Various types of bacteria can cause the infection but untreated chlamydia and/or gonorrhea are the most common.
PID is most common in women ages 15 to 25. This STD is also the leading cause of infertility in women in the United States.
While someone can acquire PID sexually, other things like douching and IUD insertion can lead to getting PID. Thankfully though, the risk of PID is only limited to the first three weeks after the IUD is inserted.
It is possible for someone to have PID and not have any symptoms. But when symptoms show, they can include dull pain in the lower abdominal area, painful urination, pain during sex, increased vaginal discharge, bleeding between periods, fever, chills, nausea, and/or vomiting.
Typically, a health professional diagnoses PID with a physical exam that verifies the tenderness of the various parts of the female reproductive system. They can also use an ultrasound to see the extent of inflammation in the reproductive system. The ultrasound can also identify the existence of abscesses, if any. If the health professional wants to rule out which bacteria is causing the PID, they can take a sample of the infected tissue to do just that. They can also schedule a laparoscopy for the patient, a surgical procedure in which the surgeon creates a small incision in the abdomen to allow a thin, flexible tube with a light on the end to view the inside of the abdominal area.
PID is usually treated with antibiotics or antimicrobial medication. In more aggressive cases of PID, the surgical removal of the affected area may occur.
9. Trichomoniasis
Trichomonas vaginalis is parasite that causes trichomoniasis. This is one of the most common sexually transmitted diseases. In fact, in 2015, there were 122 million new cases of trichomoniasis globally. Thankfully, it is also one of the most curable.
About 70% of people who acquire trichomoniasis are asymptomatic. At least, at first. It is also more common and more noticeable in women than in men. If symptoms do arise, one can experience burning or itching of the genitals, painful intercourse, and painful urination. The female reproductive tract of an infected person may produce foul-smelling “fishy” discharge as well. If an infected person is pregnant, they are at risk of giving birth prematurely. In the male reproductive system, there have been incidences of chronic inflammation of the prostate as a result of trichomoniasis that eventually led to prostate cancer. An infected person is also has an increase risk of contracting HIV.
Since going off of symptoms are not enough, a few different lab tests are possible. One includes a swab of the reproductive tract that tests for the presence of the parasite. Another is a cell culture test. Both the swab and cell culture tests have relatively low sensitivities. However, the NAAT is the most sensitive to test for the presence of the Trichomonas vaginalis parasite. The downside is that it is the most costly test.
Once diagnosed, the medical practitioner will typically prescribe the patient with the antiprotozoal and antibiotic drug called metronidazole.
10. Human papillomavirus (HPV)
Human papillomavirus (also known as HPV) is a well-known STD. So you might be wondering why I included it in this list. Well, people often discuss this sexually transmitted disease within the context of women and girls. This has given the impression to quite a number of people that HPV is an STD exclusive to women.
But that is not the case. HPV infects men, too.
Just like a woman can have genital warts or warts elsewhere on her body depending on the type of HPV, so can men. Women can be prone to cervical cancer because of HPV. Likewise, men can be prone to penile cancer because of HPV. Just like 11 and 12 year old girls are encouraged to get the HPV vaccine as a means of prevention, 11 and 12 year old boys are encouraged to do so, too. And just like “catch up” vaccines are available for women up to the age of 26, they are available for men up to the age of 21.
People get HPV via anal, oral, and vaginal transmission. Cancers can result from these transmissions with an infected person, even if the infected person shows no symptoms. According to the CDC, “HPV is thought to be responsible for more than 90% of anal and cervical cancers, about 70% of vaginal and vulvar cancers, and 60% of penile cancers.” Looking at men specifically, according to Medical News Today, “Doctors diagnose more than 42,000 HPV-related cancers every year in the United States. Roughly 18,300 of these cancers occur in men.” That is about 44% of HPV-related cancers occurring in men. Almost half.
This STD causes almost 90% of anal and cervical cancers. Find out more about this and other STDs you've probably never heard of. Click To TweetFinal Thoughts
There is a saying that goes “the more knowledge, the more responsibility.” With the knowledge about these sexually transmitted diseases and their impact on us, we are now aware of more dangers that can come with sexual activity that is not coupled with precaution. As I was researching these sexually transmitted diseases, a few reoccurring takeaways came up. They include:
- Having transparent, honest conversations with sexual partners about sexual health history (and getting tested together, even)
- Limiting your sexual partners
- Getting tested for STDs regularly
- The importance of using protection (namely, condoms)





I know i said Donovanosis was my favourite but now it might be a tie between that and Cytomegalovirus. This was highly educational. more than anything we should strive to practice safer sex and get tested frequently. like you said a number of STIs can be asymptomatic. Absolutely brilliant!
I’m glad you found it educational! I’m still tickled at the thought of having a “favorite” from a list of STDs. 😂Thanks for reading, Jo! 😊